Introduction: SARS-COV-2 pandemic has infected approximately 20 million people worldwide and more than 700.000 fatalities have been reported. Patients with malignant hematological diseases are at particular risk for unfavorable outcomes, including intensive care unit (ICU) admission, need for mechanical ventilation (MV) and death. There is paucity of data of the outcome of cancer patients with COVID-19 in low- and middle-income countries. GELL is a collaborative network of hematological centers in 13 countries in Latin America. In this retrospective study, we aimed to look at the outcome of lymphoma patients diagnosed with COVID-19 in Latin America.
Methods: This is a retrospective study including patients with a diagnosis of lymphoma and COVID-19 infection. Patients with chronic lymphocytic leukemia/small lymphocytic lymphoma were excluded from the analysis. COVID-19 diagnosis was done by RT-PCR in all but 3 patients, in whom the diagnosis was done by serology. Active disease was defined as patients with detected disease in any setting (prior to therapy, relapse) or patients currently on treatment. Survival curves were plotted using Kaplan Meier method.
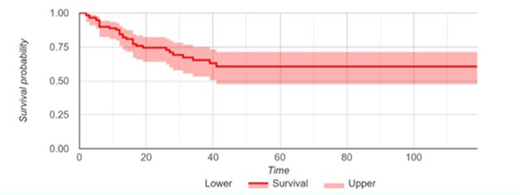
Results: A total of 117 patients were available for analysis. Median age was 60 years old, and 44% of patients had at least one comorbidity, including 32% with hypertension, 17% with obesity, 11% with cardiovascular disease and 17% with diabetes. Most patients had aggressive lymphomas (67%), including 46% of patients with diffuse large B-Cell lymphoma (DLBCL). Follicular lymphomas was observed in 13% of patients and Hodgkin's lymphoma in 10% of patients. 84% of patients had active disease, and 70% of patients were currently on treatment. With a median follow up of 17 days from COVID-19 diagnosis, 78% were admitted to Hospital, 30% needed ICU support, and 27% needed MV. Importantly, 26% of patients died, most of them within 20 days from diagnosis (Fig. 1). There was no relation between active disease (p=0.23), current treatment (p=0.65) or use of monoclonal antibodies (p=0.24) with death. COVID-19 treatment data was available in 107 patients, and 72 of them received any treatment, being steroids, the most common treatment used (n=59).
Conclusion: We confirm the dismal prognosis of patients with hematological malignancies and COVID-19 infection. In our cohort of Latin America patients with lymphoma and COVID-19, 26% of patients died with a median follow up of 17 days. No impact of current treatment or use of monoclonal antibodies were observed.
Peña:Janssen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Sandoz: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees; Amgen: Speakers Bureau; BindingSite: Research Funding. Idrobo:Amgen: Honoraria, Speakers Bureau; Abbvie: Honoraria, Speakers Bureau; Janssen: Honoraria, Speakers Bureau; Tecnofarma: Honoraria, Speakers Bureau; Takeda: Honoraria, Speakers Bureau. Abello:Novartis: Consultancy, Honoraria; Amgen: Consultancy, Research Funding; Takeda: Honoraria, Research Funding; Dr. Reddy's: Consultancy, Research Funding; Abbvie: Consultancy, Research Funding. Rojas:Novartis: Consultancy; Abbvie: Honoraria; Sandoz: Honoraria; Roche: Honoraria. Castillo:Beigene: Consultancy, Research Funding; Abbvie: Research Funding; Pharmacyclics: Consultancy, Research Funding; TG Therapeutics: Research Funding; Kymera: Consultancy; Janssen: Consultancy, Research Funding. Villela:amgen: Speakers Bureau; Roche: Other: advisory board, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal